
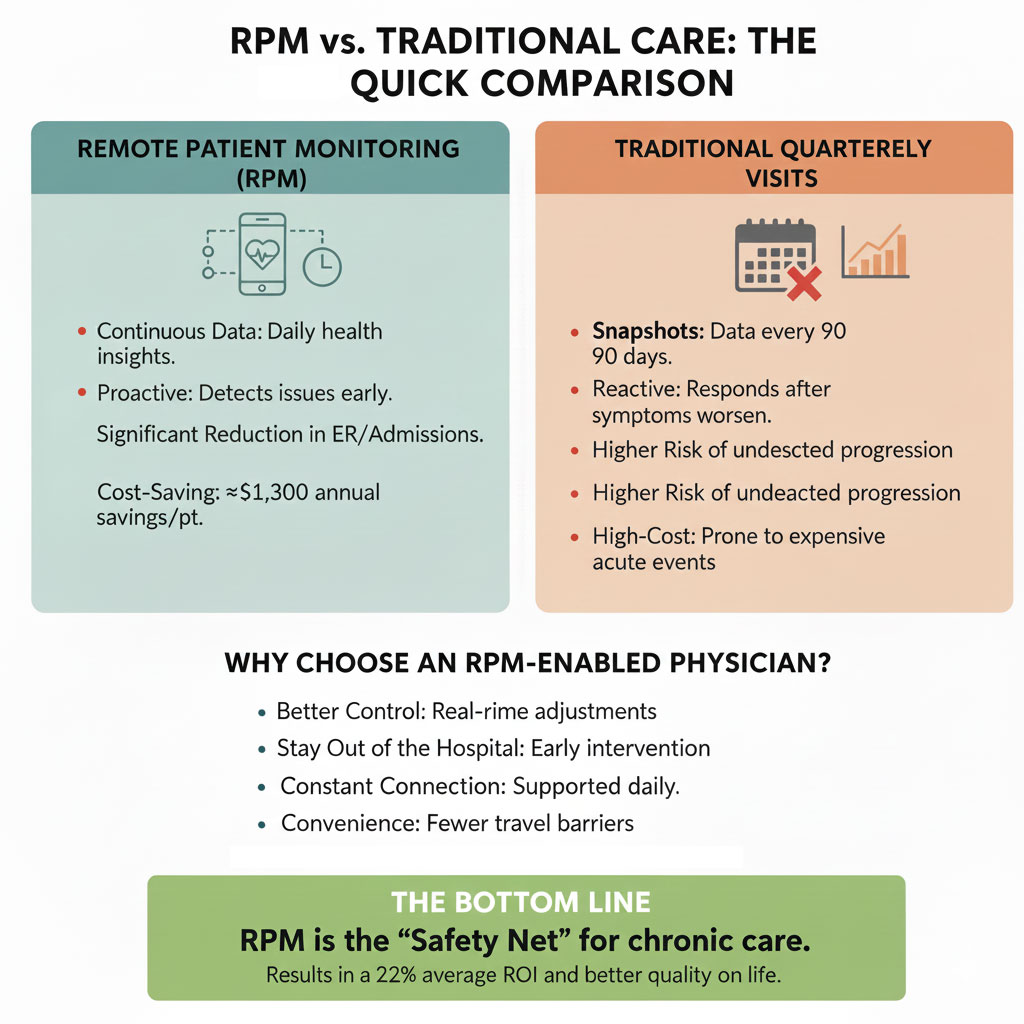
Clinical Outcomes: RPM vs Traditional Quarterly Visits
Improved Clinical Management
Studies show that RPM provides continuous data about a patient’s health – rather than just snapshots during quarterly visits – which allows clinicians to identify worsening signs before serious events occur.
• RPM is linked to reductions in hospital admissions and emergency department visits across many chronic conditions, including cardiovascular disease and COPD. Nearly half of studies on RPM report lower admissions and ED presentations compared with usual care. PubMed
• Continuous monitoring can improve disease control (e.g., better blood pressure, glucose trends) and reduce acute exacerbations because clinicians can adjust treatment based on daily data – not every 3 months. JMIR mHealth and Uhealth
Quality of Life and Satisfaction
Mortality and Severe Outcomes
In real-world settings like COVID-19 RPM programs, patients enrolled in RPM had substantially lower mortality and hospitalization rates compared with those who did not engage with remote monitoring. Mayo Clinic News Network
In contrast, with traditional quarterly visits, many early changes in disease progression go undetected for months, which can delay clinical interventions and increase risk of complications.

Return on Investment (ROI) and Cost Impact
Economic studies show that RPM is not only clinically effective but also, in many cases, cost-effective or cost-saving:
Cost Effectiveness
-
-
- Multiple systematic reviews demonstrate that RPM can be cost-effective compared with usual care, especially for conditions like hypertension, heart failure, and COPD. In cost–utility analyses, RPM has been shown to be cost-effective under typical willingness-to-pay thresholds used in health economics. PubMed+1
-
Cost Savings
-
-
- RPM programs can generate real cost savings. For example:
-
- A pandemic-related RPM program showed roughly $1,259 lower cost of care per patient in a 30-day period, mostly due to fewer and shorter hospital stays. Mayo Clinic News Network
- Health system analyses indicate RPM participation was associated with annual savings of over $1,300 per patient and significant reductions in hospital admissions. rpmleadershipcouncil.org
-
- RPM programs can generate real cost savings. For example:
-
Return on Investment (ROI)
-
-
- Some RPM economic evaluations report positive ROI, with returns such as 22.2% average ROI at realistic compliance rates. Higher compliance and efficient workflows (like automated scheduling and documentation) can push ROI even higher. circle.healthcare
-
Reduced High-Cost Events
-
-
- By preventing hospital admissions and readmissions – two of the most expensive components of chronic care – RPM helps slow the growth of healthcare costs over time. Remington Report & Home Care Education
-
RPM Changes Utilization Patterns in Favor of Better Outcomes
- Patients using RPM may have more routine outpatient contacts (remote check-ins and proactive adjustments) rather than sporadic visits every quarter. While this can appear like “more utilization,” it is typically preventive and leads to fewer severe events that require costly acute care. JMIR mHealth and Uhealth
- RPM is generally associated with lower rates of hospital admissions and shorter hospital stays outcomes that matter more for patient quality of life and cost containment than simply tracking in-clinic visit counts. PubMed
Why a Patient Should Prefer an RPM-Enabled Physician
From a policy and evidence perspective:
Better Clinical Control
RPM equips clinicians with near-real-time data that enhances decision-making and adjustment of therapy especially for chronic conditions where trends matter. Waiting months between visits risks missing early deterioration.
Proactive vs Reactive Care
RPM enables early intervention rather than waiting for symptoms to worsen until the next scheduled appointment. This reduces avoidable complications and supports steadier chronic disease management.
Improved Engagement and Adherence
Patients who are observed and engaged more frequently tend to stay more adherent to care plans, which in turn leads to better outcomes, fewer complications, and greater satisfaction.
Economic and Access Benefits
RPM can reduce the burden of travel, decrease hospital use, and produce cost savings for health systems, payers, and patients alike while still maintaining or improving health outcomes.
Summary Recommendation
Yes, for most patients with chronic conditions, choosing a physician who uses Remote Patient Monitoring (RPM) in addition to regular in-office care is associated with better outcomes and more efficient care delivery compared with a physician who only sees you every few months.
RPM advantages include:
✔ Continuous monitoring and early detection of health deterioration
✔ Lower risks of hospitalizations and acute complications
✔ Better chronic disease control
✔ Evidence of cost-effectiveness and positive ROI
✔ Higher patient satisfaction and engagement
Conclusion: When managing chronic conditions, connected care through RPM enhances physician oversight, strengthens patient engagement, and improves clinical and economic outcomes compared with traditional episodic care alone. Patients seeking optimal long-term management should strongly consider practices that integrate remote monitoring into their care model.
For more information, write to contact@medicalofficeforce.com


Impressive and important update. Thanks for the information.
Very Helpful.
RPM clears the traditional healthcare visit with a new era of instant care by monitoring the PTs.
Very informative. Thank you for sharing.
Great insight! The post clearly explains how RPM services are a win-win for both patients and physicians by supporting preventative healthcare.
This explanation is very clear and informative.
Remote Patient Monitoring allows for timely interventions and evidence based care.
RPM services offer so may great benefits, for both the patient and the provider!
Great information and quite insightful
Thank you for sharing this informative blog. Excellent insights!
Very informative.
Great ‘ RPM helps doctors track patients daily instead of waiting months between visits. This leads to better control of chronic conditions, fewer hospital visits, and improved patient satisfaction.
The message is clear, well-structured, and effectively highlights the clinical, patient-centered, and economic benefits of RPM. It positions connected care as a forward-thinking enhancement rather than a replacement for traditional care, which strengthens credibility.
Thanks for sharing this blog is very informative
very informative
Very informative.
Thanks for sharing.
Nice, It is very useful for both Physicians and the patients for the early detection of health deterioration.
Informative, Excellent
Continuous monitoring through RPM services helps prevent complications while improving both patient experience and care quality. Thanks for sharing.
Informative
Informative, Excellent comparison of RPM outcomes.
RPM is a great step forward in monitoring a patient’s chronic conditions and overall health. This informative article can help spread the word to patients who can really benefit from this program and its innovative technology. Great work!
Informative and helpful. It is great to have such important information.
“RPM is the Safety Net for chronic care management” at lower cost. Very informative and thank you for sharing.
This information is valuable for both our elderly patients and anyone with chronic conditions. By enabling early intervention, it helps reduce hospitalizations and ER visits. Very convenient since patient’s don’t need to travel or wait in long lines for a doctor visits.
Great read! This topic is invaluable!! Thanks
very clear and informative comparison showing how RPM improves clinical outcomes compared to traditional quarterly visits.
Very informative and easy to understand. Could be used as a marketing tool if it isn’t already.
great write up , let the whole worlf know that RPM if life saver and save money too.
This was a very insightful read. It clearly explains why Remote Patient Monitoring can make such a difference for people managing chronic conditions.
RPM facilitates continuous monitoring, making care more proactive and patient-friendly. Informative read!
Really helpful. Keep posting more blogs regarding the same.
informative blog, keep sharing the information regarding RPM.
Love the return of investment with RPM , better outcome at lower cost. Patients need to insist for this service. Thank you fo sharing the information